
Detailed Claims Status Information
The header of the "Detailed Claim Status Information" page provides information specific to the claim. You will also see a letter icon in the "ADR Letter" field if the claim is pending response to a request for additional documentation.
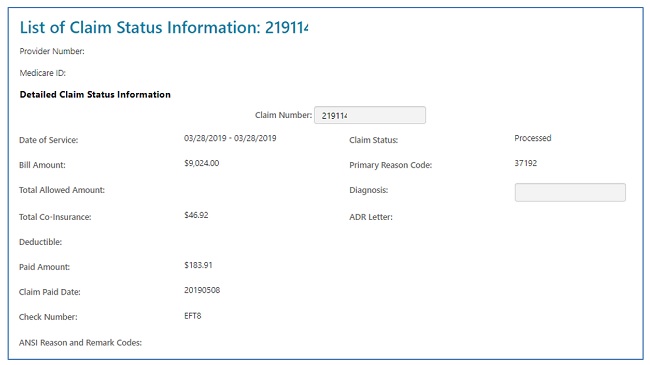
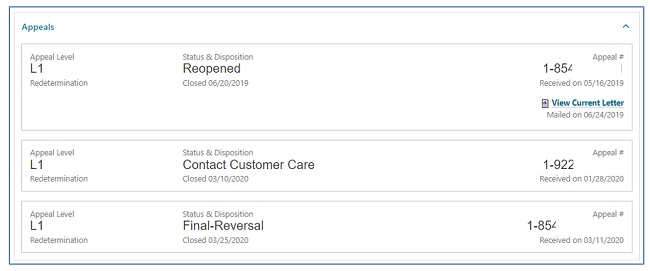
Part A and HHH claims will also display an appeals window, giving you access to appeal actions taken on claims. Not only will the status of the 1st level of the appeal (Redetermination) display, but also links to the decision letter and, if applicable, a link to request a 2nd level appeal (Reconsideration). Refer to the Appeals section of this user manual for additional information.
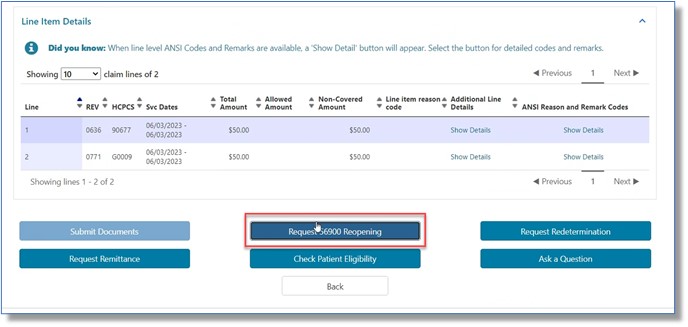
The line item details are displayed next, which includes:
- HCPCS/CPT codes
- Service dates
- Billed and allowed amounts
- Non-covered charges
- CARC and RARC codes on completed claims only (if available).
- Links will allow you to view the definition of CARC/RARC codes.
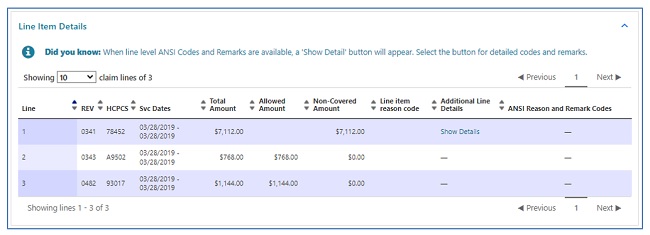
- Links will allow you to view the definition of CARC/RARC codes.
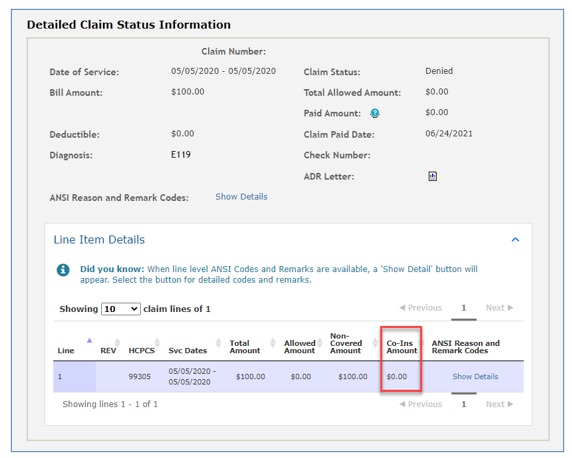
The Detailed Claim Status Information page for Part B users will not display the co-insurance information in the header, but on each detail line instead.
Depending upon the status of the claim, the date of service and/or the date the claim was processed, you may perform a number of functions directly from the status page:
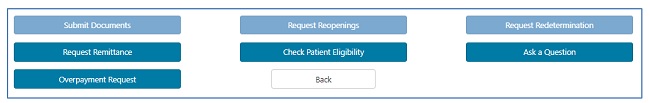
- Submit Documents: Select this option if the claim is pending due to a request for additional documentation from either our Claims or Medical Review departments.
- This allows you to attach documentation and respond to the request directly through myCGS.
- Accessing the ADR form from the Claims for Medical Review tabs will ensure the form is correctly auto-populated with the details needed to process your response.
- Refer to the Medical Review section of this user manual for help navigating the ADR form.
NOTE: When claims are pending due to an ADR, do not use the 'Ask a Question' button, as it will not route the documentation you attach to the pending claim.
- This allows you to attach documentation and respond to the request directly through myCGS.
- Request Reopening (Part B): This option allows you to submit a request for a simple correction to a Part B claim that has been processed.
- There are various types of Part B Reopenings. Refer to the Forms/Reopenings (Part B) section of this user manual for help with navigation.
- Request Redetermination: This option allows you to submit a first-level appeal directly through the portal and include any documentation you have to support your case.
- Refer to the Appeals section of this user manual for help with navigation.
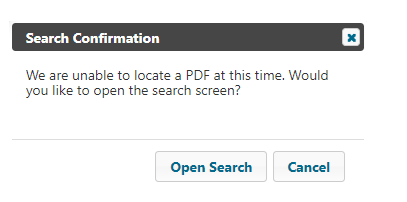
- Request Remittance: Select this option to review and/or print a copy of a remittance advice.
- When clicking the Remit button from the claims detail page, if there is a single remit associated with the claim, then the remit will automatically open. If associated with several remits, a popup will ask the user if they would like to open the Remit Search Screen
- Refer to the Remittance section of this user manual for navigation assistance.
- When clicking the Remit button from the claims detail page, if there is a single remit associated with the claim, then the remit will automatically open. If associated with several remits, a popup will ask the user if they would like to open the Remit Search Screen
- Check Patient Eligibility: Selecting this option will open the “Eligibility” tab, allowing you to view details specific to the patient, including status, deductible, preventive services, secondary status, and Medicare Advantage (MA) Plan enrollment.
- Refer to the Eligibility section of this user manual for additional information.
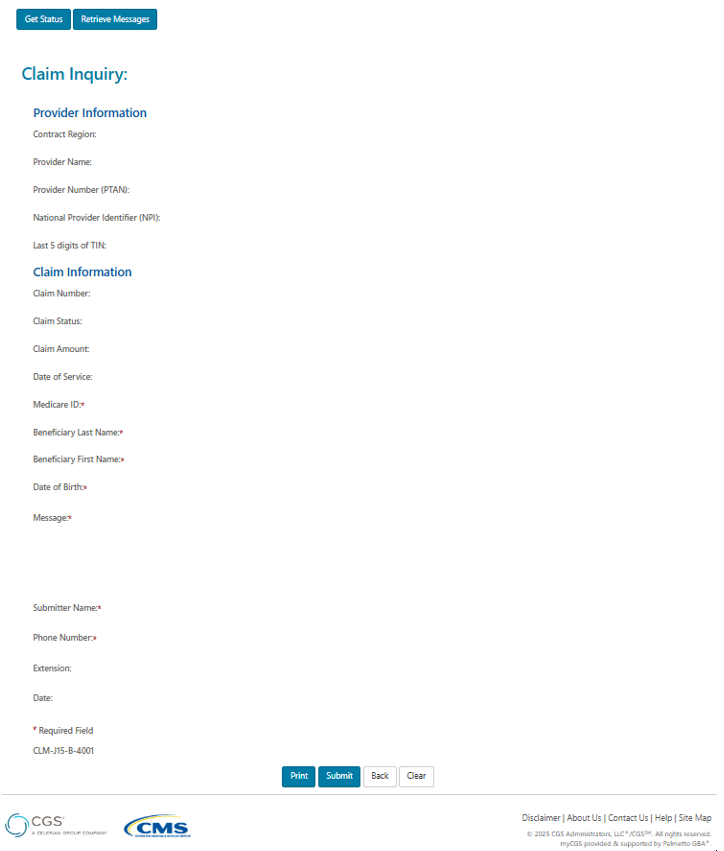
- Ask a Question: This option will allow you to submit a general question regarding the claim. Status Inquiries are not to be submitted for "Ask a Question."
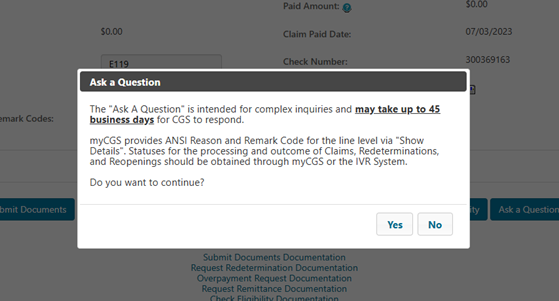
Please remember “Ask a Question” is not used for claim status inquires, but only for complex inquiries and may take up to 45 business days for a response.
After selecting Yes, please complete all the fields and place your complex inquiry in the message field. Then click submit.
- Overpayment Request: Select this option if the claim was billed in error and you need an overpayment letter generated to request the funds be returned.
- 56900 Reopening (A/HHH Claims Only): For Part A, Home Health, and Hospice claims, users may submit a 56900 Reopening when a claim has denied for non-response to an ADR (reason code 56900). When this situation is present (after 45 days but within 120 days), the option to submit the request will display on the List of Claims page and at the very bottom of the Detailed Claim Status Information page.
For your convenience, when you select one of the functions noted above, you will be routed to the applicable online form. Most of the required fields on the form will auto-populate with information from the claim and specific to your User ID.
NOTE: Options above that are not available for the claim displayed will be grayed out. Grayed options could also indicate you do not have authorization to perform that function. Check with your Provider Administrator for access.
You may also click "Back" to return to the claim list.


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn