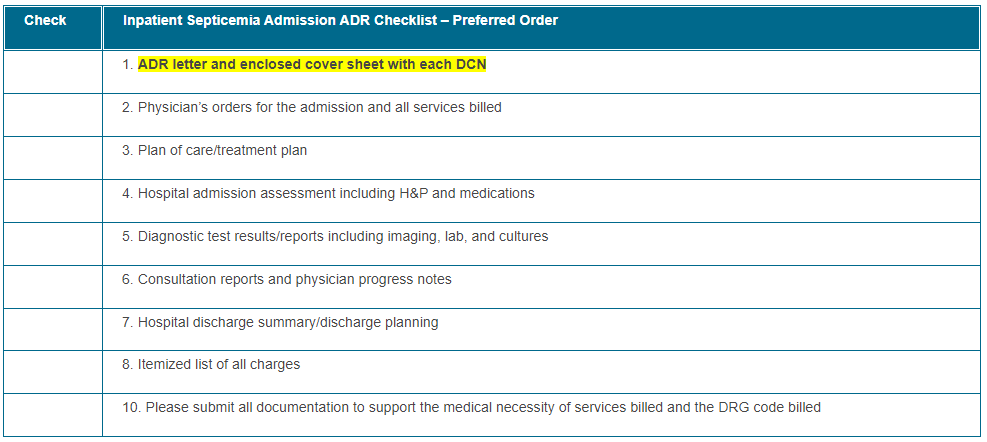
Inpatient Septicemia ADR Checklist
CGS recommends providers organize the medical documentation in the order indicated below. This will assist CGS in reviewing your documentation more efficiently, and will expedite the review process. Please ensure the documentation is submitted within 45 days of the Additional Documentation Request (ADR). If the documentation has not been received, the claim will automatically deny on the 46th day for non-receipt of documentation.
Providers should submit all documentation that is pertinent to support the medical necessity of services for the billing period being reviewed. Ensure services billed are coded accurately for the service provided and the documentation supports those services. This may include documentation that is prior to the review period. Please note that the most common reason for overturned appeals are due to providers submitting new documentation upon the appeal that was omitted with the initial submission of medical records.
*Please include the beneficiary name and date of service on all documentation and include an abbreviation key (if applicable). Documentation must be legible and complete (including signature(s) and date(s)). If you question the legibility of your signature, you may submit a signature log or an attestation statement.
The Checklist below is intended to be utilized by providers as a reference when responding to Additional Documentation Requests (ADR) to ensure each claim meets the policy requirements prior to the ADR submission. Please submit all documentation as required in the LCD or NCD if applicable and in accordance with the Medicare Benefit Policy Manual. It is the responsibility of the provider to submit complete and accurate documentation per the regulatory guidelines for each claim. Ensure the documentation submitted belongs solely to the intended beneficiary and documentation of another beneficiary is not present within any aspect of the medical record.
Click on the table below for a printable version.
Helpful Links:
- CMS Medicare Learning Network website

- CGS Administrators, LLC J15 Part A website
- CGS Administrators, LLC J15 Part A website (educational materials)
- CMS Medicare Program Integrity Manual: (Pub. 100-08), Chapter 3, Section 3.3.2.4

- CMS MLN Matters Article MM6698: Signature Guidelines for Medical Review Purposes

- Complying with Medicare Signature Requirements MLN905364 – Complying with Medicare Signature Requirements (cms.gov)

- Definition of "medically necessary": Social Security Act (SSA), Section 1862 (a)(1)(A)

- Code of Federal Regulations: Electronic Code of Federal Regulations

How to Prevent Common Denials:
Ensure Documentation includes:
- Documentation to support the medical necessity of the services billed
- Hospital admission assessment and H&P
- Diagnostic test results/reports including imaging, labs, and cultures
- Clear documentation of sepsis diagnosis present on admission
Please visit:
Providers may include an outline or cover letter with their documentation. This can be used by CGS Medical Review staff as an Index, and prove very helpful to provide the location of key documentation that supports payment of the claim. However, the cover letter cannot be used as documentation, and the documentation must support the contents of the cover letter in order to be useful.
In addition, providers may use brackets, such as [ ] or { }, asterisks (*) or underlined text in the documentation to draw the reviewer's attention to important information. However, notations should not alter, or give the appearance of altering, the documentation. The use of a highlighter is not recommended as documentation may not be legible.
We encourage all CGS providers to utilize myCGS Portal, a free service available 24/7, which offers access to beneficiary eligibility, claim and payment information, forms allowing you to submit redetermination requests, and respond to Medical Review Additional Documentation Requests (ADRs) and much more. Please enroll for myCGS if you have not already done so.
Check the Calendar of Events to sign up for any webinars that may be of interest.
Please contact J15AMREDUCATION@cgsadmin.com for further questions, concerns, or educational needs related to the TPE process. Be sure to include the facility name and Provider number/PTAN for the inquiry. Ensure CGS is current with provider contact information for any educational outreach opportunity.