
Plan Coverage
The "Plan Coverage" sub-tab provides information regarding the beneficiary's enrollment under Medicare Advantage (MA) Managed Care Plans (commonly referred to as Part C contracts) that provide Part A and B benefits for beneficiaries.
This sub-tab also provides information on a beneficiary's Part D prescription drug coverage.
NOTE: Whenever myCGS indicates that a beneficiary has coverage through a non-Medicare entity (MA or Medicare Drug Benefit plans), the inquiring provider should always contact the non-Medicare entity for complete beneficiary entitlement information.
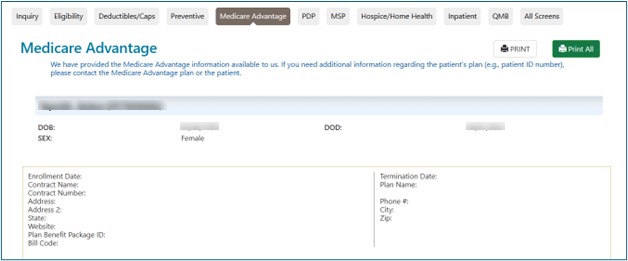
The table below describes the "Plan Coverage" sub-tab fields:
| Field Name | Description |
|---|---|
Plan Type |
A full plan description followed by Plan Type Code:
|
Enrollment Date |
The date that indicates the start of enrollment to the coverage plan |
Disenrollment Date |
The date that indicates the termination of enrollment to the coverage. No date in this field means the plan enrollment has not terminated. |
Contract Name |
A descriptive name of the beneficiary's insurance coverage organization |
Contract Number |
The contract number (if on file) |
Address |
The coverage plan's address line 1 |
Phone Number |
The coverage plan's contract telephone number (if on file) |
Address 2 |
The coverage plan's address line 2 |
City |
The coverage plan's city |
State |
The coverage plan's state |
ZIP Code |
The coverage plan's ZIP code |
Website |
The coverage plan's website address that will provide information on the beneficiary's insurance |
Bill Code |
The bill code of the plan type. This field only applies to plan types HM, HN, IN, PR, and PS. Medicare Beneficiary "locked in" to MCO Medicare Beneficiary NOT "locked in" to MCO |


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn