<< Return to the full list of Part B FAQ topics
Click on an item to expand or Show All / Close All
1. When using time to choose level of service, how should that be documented?
Total time may be documented as a whole; however, best practice includes documenting the specific activities with the time spent performing them. The documentation should support the time reported.
| Published | 02/xx/2021 |
2. G2211 - what specialties can bill and what documentation is required?
HCPCS code G2211 is an add-on for visit complexity that may be used with MDM or Total Time in office or other outpatient E/M services. CMS is not restricting billing based on specialty. The documentation must support the detailed and high level of complexity in addressing the broad scope of the patient's healthcare needs. CGS is anticipating further guidance from CMS.
| Published | 02/xx/2021 |
3. What time ranges does CMS expect providers to use to report 99202-99215 based on time?
CMS has aligned with the new AMA time frames for codes 99202-99215. These times are always subject to CMS approval. Reference: https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf![]()
| Published | 02/xx/2021 |
4. If Telehealth will be continued under the Cares Act what is the guidelines for other insurance carriers?
Please Reference the CMS Current Emergencies for MA Plans under "Read our provider-specific fact sheets on new waivers and flexibilities at https://www.cms.gov/about-cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-waivers
| Published | 02/xx/2021 |
5. For external review of documents from a unique source - what does CGS consider a unique source?
Data to be reviewed and analyzed may include prior external records, communications and/or test results are from an external physician, other qualified health care professional, facility or healthcare organization. An external physician or other qualified health care professional is an individual who is not in the same group practice or is a different specialty or subspecialty. Reference: https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf![]()
| Published | 02/xx/2021 |
6. Please clarify pulling forward chronic conditions that pertain to the specialist's care, but they may not be managing.
Noting chronic conditions, that another specialist manages, in the patient's medical record does not alone qualify as being a problem addressed. Reference: https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf![]()
| Published | 02/xx/2021 |
7. Are there office/outpt services that should continue to use 95/97 E/M guidelines rather than new 2021 MDM or Time guidelines?
For office or other outpatient E/M services, the 1995 and 1997 guidelines will no longer be used; rather, the provider may choose to use MDM or Total Time in determining the appropriate level of service code.
| Published | 02/xx/2021 |
8. Detailed examples of different types of imaging ordered, reviewed, and independent interpretations - and how they are scored.
Please see the following table for category examples of 'Amount and/or Complexity of Data to be Reviewed and Analyzed. Reference: https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf![]()
| Published | 02/xx/2021 |
9. With all the issues brought on by COVID 19, is there any hope on the horizon that Congress will repeal MIPS?
Not at this time, please continue to review the Current Emergencies and Flexibilities at https://www.cms.gov/about-cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-waivers![]()
| Published | 02/xx/2021 |
10. Specific updates relating to substance use disorder services
Please visit the CMS website for 2021 updates at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Opioid-Treatment-Program![]()
Published |
02/xx/2021 |
11. 99072 - is this payable during the PHE?
CMS issued MLN MM11939 to identify that the CPT Code 99072 is a Status B code. This code is not reimbursed by Medicare
| Published | 02/xx/2021 |
12. Would an OARRS check be considered an external review of documents from a unique source under data or is this considered part of the RX management under the risk?
If the Rx history report is intentionally requested and used in the providers MDM, it may be considered an external review from a unique source. If this is a routine order per state requirement, practice policy, etc., it would not be considered.
| Published | 02/xx/2021 |
13. Does time or MDM trump the other? If MDM is higher than the time documented can MDM trump the time documented? Can we give credit for whatever is higher? of course medically necessary ?
The documentation must support the medical necessity of the services provided; either MDM or Total Time may be used to choose the level of service for office or other outpatient E/M visits.
| Published | 02/xx/2021 |
14. Is CMS/CGS going to follow AMA times for cpt codes 99212-99205?
CMS has aligned with the new AMA time frames for codes 99202-99215. These times are always subject to CMS approval.
| Published | 02/xx/2021 |
15. Does CGS consider doing testing on a patient taking anticoagulants as meeting the definition of drug therapy requiring intensive monitoring for toxicity?
When routine testing is performed for patients taking anticoagulants and the results require significant action, it may be considered intensive monitoring with follow up.
| Published | 02/xx/2021 |
16. For complexity of data can you count one point for ordering a test and count a point at next visit for reviewing results?
The AMA states, "Ordering a test and the review of the test result is part of the encounter and not a subsequent encounter."
| Published | 02/xx/2021 |
17. Can the order of a unique test be counted for Category 1 if the test was performed and billed for on the date of service?
The AMA states, "Ordering a test and the review of the test result is part of the encounter and not a subsequent encounter," however, the test is not included when choosing a level of service if the physician is the performing and billing entity.
| Published | 02/xx/2021 |
18. What code is used by Medicare for extended services and what is the time breakdown for units?
CMS finalized the HCPCS code G2212 for prolonged office/outpatient E/M services when selecting total time.
G2212: Prolonged office or other outpatient evaluation and management service(s) beyond the maximum required time of the primary procedure which has been selected using total time on the date of the primary service; each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact
Add-on code, list separately in addition to CPT codes 99205, 99215 for office or other outpatient evaluation and management services
Do not report G2212 on the same date of service as 99354, 99355, 99358, 99359, 99415, 99416
Do not report G2212 for any time unit less than 15 minutes
Effective January 1, 2021
Tables listing the codes and total time required for reporting may be located in the MLN Matters MM12071![]() .
.
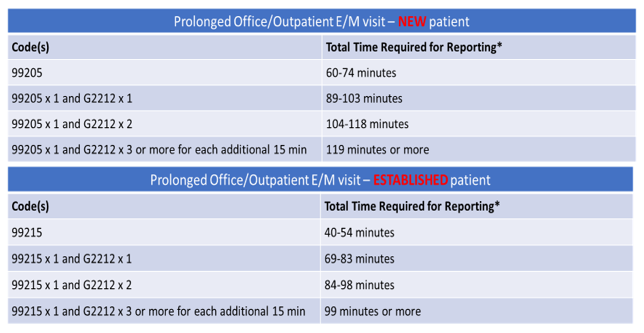
*Total time is the sum of all time, with and without direct patient contact and including prolonged time spent by the reporting practitioner on the date of service of the visit.
| Published | 02/xx/2021 |
19. Can residents bill G2211 under primary care exception?
The use of HCPCS code G2211 (visit complexity) has been delayed and will be unavailable until further notice from CMS.
Resident work is billed under the supervising/teaching physician's PTAN with the primary care exception and must meet CMS regulations, coding, and billing guidelines. Under the primary care exception the teaching physician may direct the care furnished by the resident and review the services furnished by the resident during or immediately after the visit, remotely using audio/video real-time communications technology. When the resident and teaching physician collaborate, the time may only be counted once toward total time or total MDM.
Published |
02/xx/2021 |
20. Are all tests including labs billed by the same office the provider is in restricted from being counted towards data in MDM?
If the provider is getting paid for the test, they cannot include it when choosing the level of E/M service also.
The AMA states, "Any specifically identifiable procedure or service (ie, identified with a specific CPT code) performed on the date of E/M services may be reported separately.
The actual performance and/or interpretation of diagnostic tests/studies during a patient encounter are not included in determining the levels of E/M services when reported separately."
Published |
02/xx/2021 |
21. G2211? Why is it delayed?
The use of HCPCS code G2211 (visit complexity) has been delayed and will be unavailable until further notice from CMS. Funding for code G2211 has been allocated elsewhere for physicians.
Published |
02/xx/2021 |
22. What CMS source document includes the finalized E&M times CMS will use in 2021?
The most recent publishing from CMS is the MLN Matters MM12071![]() which includes the total time required for reporting codes 99205, 99215, and G2212.
which includes the total time required for reporting codes 99205, 99215, and G2212.
Published |
02/xx/2021 |
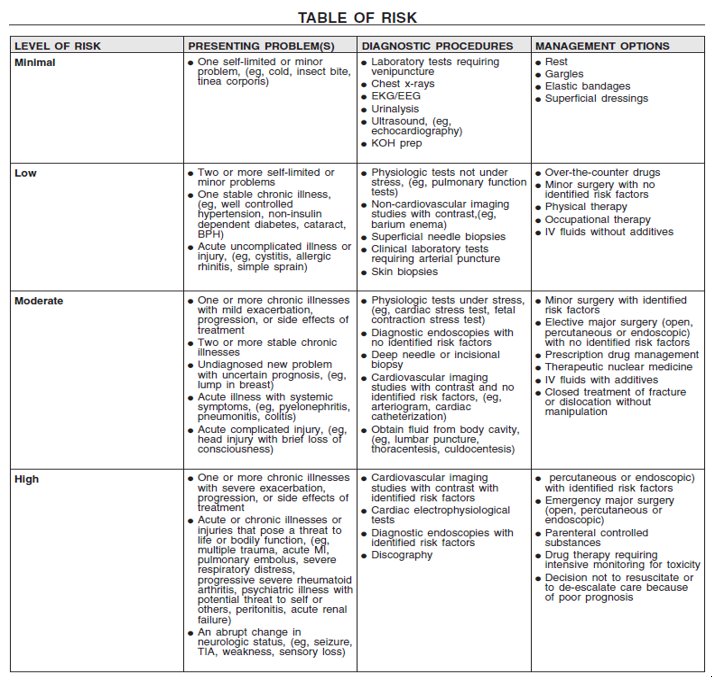
23. How do you define "minor" and "major" procedures in the MDM/risk column? Can you give examples?
Minor and major procedures may be based upon the patient's and procedure's risk factors. The type of anesthesia is also a consideration, examples include local anesthesia, conscious sedation or general anesthesia. The determination should be clearly documented by the physician in the medical record.
Defining Risk
The AMA defines risk as: "The probability and/or consequences of an event.
The assessment of the level of risk is affected by the nature of the event under consideration.
For example, a low probability of death may be high risk, whereas a high chance of a minor, self-limited adverse effect of treatment may be low risk.
Definitions of risk are based upon the usual behavior and thought processes of a physician or other qualified health care professional in the same specialty.
Trained clinicians apply common language usage meanings to terms such as 'high', 'medium', 'low', or 'minimal' risk and do not require quantification for these definitions, (though quantification may be provided when evidence-based medicine has established probabilities).
For the purposes of medical decision making, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated. Risk also includes medical decision making related to the need to initiate or forego further testing, treatment and/or hospitalization."
Published |
02/xx/2021 |
24. Focus on data and how/when to count data, order and review of testing. Giving examples would be helpful.
The AMA states, "Ordering a test and the review of the test result is part of the encounter and not a subsequent encounter."
Example: If you order a CBC on the date of service and review the results at a later follow up with the patient, the order and review are only included on the first date of service.
Published |
02/xx/2021 |
25. If a PCP reviews the notes of a cardiologist under the same TIN as the PCP - can that credited as review of prior external note?
Yes, this may be included in Category 1 of the Elements of Medical Decision Making table since the cardiologist is a different specialty.
The AMA provides the following definition: "An external physician or other qualified health care professional is an individual who is not in the same group practice or is a different specialty or subspecialty. It includes licensed professionals that are practicing independently. It may also be a facility or organizational provider such as a hospital, nursing facility, or home health care agency."
Published |
02/xx/2021 |
26. Could you provide an example of the extended visit 99356 in a hospital setting for physician?
CPT code 99356 does not apply to the new 2021 office/other outpatient E/M service changes.
CPT code 99356 is a prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service; first hour. This code would be listed separately in addition to the code for inpatient or observation E/M services.
Published |
02/xx/2021 |
27. When a provider is ordering/interpreting and billing for the global x-ray, does the physician get credit under MDM for this?
If the provider is getting paid for the test, they cannot include it when choosing the level of E/M service.
The AMA states, "Any specifically identifiable procedure or service (i.e., identified with a specific CPT code) performed on the date of E/M services may be reported separately. The actual performance and/or interpretation of diagnostic tests/studies during a patient encounter are not included in determining the levels of E/M services when reported separately."
Published |
02/xx/2021 |
28. If you order 3 separate/unique coded CPT tests do you meet the Category 1 criteria for level 4 or 5?
The AMA provides the following definition: "Tests are imaging, laboratory, psychometric, or physiologic data. A clinical laboratory panel (e.g., basic metabolic panel [80047]) is a single test. The differentiation between single or multiple unique tests is defined in accordance with the CPT code set."
The three different unique tests may fulfill Category 1 for Amount and/or Complexity of Data to be Reviewed and Analyzed; however, there are still other requirements to be met when determining the level of service.
Published |
02/xx/2021 |
29. Can we combine the 95/97 documentation guideline risk table management options with the 2021 risk/patient management options?
Please see the Table of Risk located in the 2021 CPT Book edition. For office/other outpatient E/M services, the 1995 and 1997 E/M guidelines will no longer be used.
Published |
02/xx/2021 |
30. Can you clarify what is considered as analyzing and interpreting a lab? Provider did not bill for it.
An example would be a practitioner who reviews chest x-ray films or EKG strips to determine the interpretation/result.
The AMA defines independent interpretation as: "The interpretation of a test for which there is a CPT code and an interpretation or report is customary.
This does not apply when the physician or other qualified health care professional is reporting the service or has previously reported the service for the patient.
A form of interpretation should be documented, but need not conform to the usual standards of a complete report for the test."
31. If they continue to just maintain a medication and the patient's condition is controlled(stable) would this fall under that Moderate Decision Making criteria for you level 4 visits. Or this just simply be under management of a medication?
Prescription drug management includes a dosage increase or decrease (or the addition of a new medication) based upon clear documentation of a problem addressed and data reviewed for patient management; however, there are other requirements to meet a level Please see the AMA's Elements of Medical Decision Making table.
For 2021 office or other outpatient E/M services, the following elements are considered when determining the level of MDM.
Number and Complexity of Problems Addressed
Amount and/or Complexity of Data to be Reviewed and Analyzed
Risk of Complications and/or Morbidity or Mortality of Patient Management
Published |
02/xx/2021 |
32. Clarification for definition of "independent historian" – would this include parent of a patient that is very young and unable to give history on their own? I know there's not a lot of pediatric patients; however, there is the occasion, so if we have a 2 year old that is too young to give history, would you allow the parent to count as independent historian?
The AMA provides the definition of an independent historian which includes the parent of a child who is unable to provide a complete or reliable history due to their developmental stage.
Published |
02/xx/2021 |
33. Patient has KUB at hospital and brings films (CD) and report to our office. We see the patient and look at the report and films, can we get 1 pt for reviewing data and a point for the independent interpretation of test performed by other professional? We are reviewing data and interpreting that data.
The AMA defines Independent Interpretation as: "The interpretation of a test for which there is a CPT code and an interpretation or report is customary. This does not apply when the physician or other qualified health care professional is reporting the service or has previously reported the service for the patient. A form of interpretation should be documented, but need not conform to the usual standards of a complete report for the test."
The AMA also reports, "Ordering a test is included in the category of test result(s) and the review of the test result is part of the encounter and not a subsequent encounter."
In the Elements of Decision Making table, Category 2 requires an Independent interpretation of a test performed by another physician/other qualified health care professional (not separately reported).
Therefore, the scenario in question depends on several other variables: If the physician ordered the KUB and the patient brings a CD with report (interpretation) to the office, this would have been counted as ordering/review of the results of a unique test. If the physician did not order the KUB, it would be considered a review of prior external notes from a unique source.
Published |
02/xx/2021 |
34. This scenario is popping up for cardiology patients. We are a large, multi-specialty group, with cardiologists, interventional cardiologists, vascular surgeons, and cardiothoracic surgeons.
A patient with multiple cardiology problems may have a diagnostic test (i.e., TEE) performed by Dr. Smith on 01/04/21. Dr. Smith will perform, interpret and bill (93314).
Dr. Jones will review the TEE results at a patient appointment on 01/11/21.
May Dr. Jones count his review of the TEE as a data point in his MDM for the E/M on 01/11/21? It seems unfair to Dr. Jones if we can't count the TEE because it was paid to Dr. Smith (a partner on his team) on 01/04/21.
I hope we are overthinking and the only procedures we can't count are ones done on the same calendar day. Since the physician's bill under the same Tax ID, we aren't sure how this scenario would be counted.
The AMA provides the following definition: "An external physician or other qualified health care professional is an individual who is not in the same group practice or is a different specialty or subspecialty. It includes licensed professionals that are practicing independently. It may also be a facility or organizational provider such as a hospital, nursing facility, or home health care agency."
The documentation must support the Medical Decision Making from Dr Jones and how he used the results of the TEE. For 2021 office or other outpatient E/M services, the following elements are considered when determining the level of MDM.
Number and Complexity of Problems Addressed
Amount and/or Complexity of Data to be Reviewed and Analyzed
Risk of Complications and/or Morbidity or Mortality of Patient Management
The physician may also choose the level of service based on Total Time.
Published |
02/xx/2021 |
35. When documenting total time in the progress note, may a time range (e.g. 10-19 minutes) be documented instead of an exact time (e.g. 16 minutes)?
Though code descriptions identify a time range for billing purposes, providers must document exact times. Total time may be documented as a whole (16 minutes); however, best practice includes documenting the specific activities with the time spent performing them. The documentation should support the time reported.
Published |
02/xx/2021 |
36. Does Medicare allow shared office visits?
Per the AMA CPT: "A shared or split visit is defined as a visit in which a physician and other qualified health care professional( s) jointly provide the face-to-face and non-face-to-face work related to the visit. When time is being used to select the appropriate level of services for which time-based reporting of shared or split visits is allowed, the time personally spent by the physician and other qualified health care professional( s) assessing and managing the patient on the date of the encounter is summed to define total time. Only distinct time should be summed for shared or split visits (i.e., when two or more individuals jointly meet with or discuss the patient, only the time of one individual should be counted)."
Medicare allows shared/split visits in the hospital setting and "incident to" visits in the office setting that meet CMS regulations, coding, and billing requirements.
Please see the following resource with references for "incident to" visits and Split and Shared Care:
Published |
02/xx/2021 |
37. If a practitioner orders, performs and interprets an EKG during an E/M office visit and bills CPT 93000 in addition to the E/M office visit CPT, does ordering the EKG count as a data element in the medical decision making (MDM) table/grid for determining the E/M office visit CPT level?
The AMA states, "Any specifically identifiable procedure or service (ie, identified with a specific CPT code) performed on the date of E/M services may be reported separately. The actual performance and/or interpretation of diagnostic tests/studies during a patient encounter are not included in determining the levels of E/M services when reported separately. If a test/study is independently interpreted in order to manage the patient as part of the E/M service, but is not separately reported, it is part of medical decision making."
Published |
02/xx/2021 |
38. Is it required to state in a progress note for an office visit whether the patient is considered new versus established?
The code selected for the level of E/M service is going to be different for new and established patients. It is not a requirement to state in the progress note whether the patient is new or established; however, this would be considered best practice.
Published |
02/xx/2021 |
39. Birth Weight Checks for Peds Office - Using MDM we get straightforward MDM but providers say MDM should be Low due to the amount of Risk but there are not other orders or complexity of problems addressed. Since the baby is not gaining weight can I use the Acute illness with systemic symptoms since the babies are newborns? Thank you for any guidance.
Based on the scenario provided, the MDM would be straightforward. The Elements of Medical Decision making table needs to be applied with focus on the problems addressed at the encounter, data reviewed and analyzed, and patient management.
Published |
02/xx/2021 |
40. Do we still use 95/97 guidelines for IP E/M or do we only use 2021 risk table for ALL E/M now?
The 95/97 guidelines still apply to Inpatient E/M services. For office or other outpatient E/M services on or after January 1, 2021, the 1995 and 1997 guidelines will no longer be used; rather, the provider may choose to use MDM or Total Time in determining the appropriate level of service code.
Published |
02/xx/2021 |
41. Is the GPC1X code the same as the G2211?
Yes, G2211 was formerly referred to as GPC1X.
Published |
02/xx/2021 |
42. Can a history of malignant melanoma be considered in the MDM?
Yes, a history of malignant melanoma may be considered if the provider clearly documents how they are addressing and managing the problem in their MDM.
Published |
02/xx/2021 |
43. On slide 25 a question is posed regarding Prescription Drug Management. The response is not quoted from the AMA, nor have even the previous 95/97 guidelines instructed that prescription drug management only applies to a change/add of a prescription drug. The analysis of a patient's medication regimen is the same regardless of whether a decision to make a change ultimately is made. The decision to continue a medication at the same level is still management of a prescription. I do not see that the AMA has defined it in the manner you have. Can CGS please review this point again with the AMA and issue some clarification?
The medical decision making to adjust any prescription medication when addressing and managing a problem or disease requires a higher complexity than refilling or continuing a medication; therefore, the documentation must be clear and concise when describing why a prescription medication was changed or continued. Simply providing a list of the patient's medications or stating 'reviewed' would not be considered prescription drug management complexity.
Published |
02/xx/2021 |
44. When a provider orders a test for a patient at a visit but the patient does not get the tests performed and so at the follow up visit the provider orders the tests again does the order count toward data calculation for both these visits?
The scenario posed has multiple unstated elements that affect the determination of level of service.
Technically, if the original order/review was included in determining the E/M level of service on the prior date, then it would not be included in the subsequent visit even if the same test needed to be reordered.
The provider may also use qualifying factors in Total Time on the date of the encounter when choosing the level of service.
Published |
02/xx/2021 |
45. Is there a Time limit for giving Provider credit for Reviewing unique Testing? information. I have audited documentation where the Provider pulled every xray, MRI ,Ct Scan the patient had since 2013 to the present.
If the provider has not received payment for review of those tests previously, it may be included in the providers Total Time if it was medically necessary to review those tests and they are used to address a current problem.
Published |
02/xx/2021 |
46. Can we circle back to the prescription drug management, as we have this definition, any chance we can consider this for Ohio as Florida has this interpreted? Last Modified: 10/1/2020 Location: FL, PR, USVI Business: Part A, Part B.
What constitutes prescription drug management? During an evaluation and management visit, what constitutes "prescription drug management?"
"Prescription drug management" is based on documented evidence that the provider has evaluated medications as part of a service, in relation to the patient. This may be a prescription being written or discontinued, or a decision to maintain a current medication/dosage.
Note:Simply listing current medications is not considered "prescription drug management." https://medicare.fcso.com/faqs/answers/0324049.asp![]()
The medical decision making to adjust any prescription medication when addressing and managing a problem or disease requires a higher complexity than refilling or continuing a medication; therefore, the documentation must be clear and concise when describing why a prescription medication was changed or continued. Simply providing a list of the patient's medications or stating 'reviewed' would not be considered prescription drug management complexity.
Published |
02/xx/2021 |
47. To clarify the table of risk included within your slide may be utilized for determining the risk towards the MDM? Example - 2 stable chronic conditions along with continuing current treatment (either prescriptions or diet/exercise). Would this support level 4 billing?
MDM is based on the problems addressed, data reviewed and analyzed, and patient management that is Clearly documented to support the medical necessity of the visit. Two out of the three elements of MDM must be met to choose the level of service.
Published |
02/xx/2021 |
48. Prescription drug management: There does not have to be a change in dosage, starting/stopping of a prescription drug in order to give credit on the Risk Table.
A decision to maintain the current medication is sufficient.
Credit is given as long as the documentation clearly indicates that decision-making took place in regard to the medication(s). https://medicare.fcso.com/FAQs/140855.asp![]()
The medical decision making to adjust any prescription medication when addressing and managing a problem or disease requires a higher complexity than refilling or continuing a medication; therefore, the documentation must be clear and concise when describing why a prescription medication was changed or continued. Simply providing a list of the patient's medications or stating 'reviewed' would not be considered prescription drug management complexity.
Published |
02/xx/2021 |
49. Did I hear correctly that major/minor procedures pertains to whether its a major or minor risk and not a major or minor procedure?
The provider needs to assess and clearly document the patient's individual risk factors along with the procedure's risk factors to determine the overall risk. The risk determination is also based upon the "usual behavior" of a physician or QHP within that specialty.
Published |
02/xx/2021 |
50. Can residents providing care under the Primary Care Exception bill based on time and/or MDM for 99202-99215 office visits? I can find no guidance on this. Thank you !
42 CFR, § 415.174 Exception: Evaluation and management services furnished in certain centers. This exception for services furnished in outpatient departments of a hospital or another ambulatory care entity includes time spent by residents in patient care activities may be included in the level of service when specified conditions are met. https://www.law.cornell.edu/cfr/text/42/415.174![]()
Published |
02/xx/2021 |
51. If you bill for the TC of a test but not the PC, can you count the review of those images as data?
No, if the provider is the billing entity, they may not include it when choosing the level of service based on MDM.
Published |
02/xx/2021 |
52. If a dermatologist has a established patient presenting for full body skin exam and finds a wart, mole and a suspicious lesion and decides to remove the lesion for pathology, for MDM can they consider "undiagnosed new problem" if they are also billing for the biopsy removal on the same day?
When billing for the biopsy removal on the same date of service as the visit, a separate and significant problem would need to be addressed and managed in order to bill for an E/M with modifier 25.
Published |
02/xx/2021 |
53. If a provider reviews lab on a visit, how are we to know that they previously received credit for review/order from a previous visit?
Each provider's office will need to evaluate their internal processes to manage coding and billing.
Published |
02/xx/2021 |
54. Can you clarify the question on "ordering a lab"…the answer indicated if we were billing for the lab, we couldn't include that in the code level to determine the overall code. Is that correct?
When the lab or imaging is performed and billed by the provider's office, it cannot be included when selecting an E/M level of service. However, the physician may choose the level of service based on qualifying factors of Total Time.
| Published | 02/xx/2021 |
55. How is it that we can count the ordering of a test and the review of said test on the day it's ordered, but if the test is not reviewed that same day that we cannot count the review on the day it's reviewed?
The AMA, which CMS has aligned with, clearly states, "Ordering a test is included in the category of test result(s) and the review of the test result is part of the encounter and not a subsequent encounter.
Published |
02/xx/2021 |
56. Since 99211 is being eliminated, what code should be used for a RN visit? Ex: follow-up to new chemo treatment or pt needs more education on meds, etc.
Medicare does not reimburse a patient visit who only sees an RN; rather the provider would need to be involved.
Published |
02/xx/2021 |
57. Clarification, in order for the provider to receive credit for RX drug management, they must stop, start or change dosage?
The medical decision making to adjust any prescription medication when addressing and managing a problem or disease requires a higher complexity than refilling or continuing a medication; therefore, the documentation must be clear and concise when describing why a prescription medication was changed or continued.
Simply providing a list of the patient's medications or stating 'reviewed' would not be considered prescription drug management complexity.
Published |
02/xx/2021 |
58. In the 2021 E/M MDM table, RISK column… can clarification be provided on definitions for "major" and "minor" procedures?
The provider needs to assess and clearly document the patient's individual risk factors along with the procedure's risk factors to determine the overall risk. The risk determination is also based upon the "usual behavior" of a physician or QHP within that specialty.
Published |
02/xx/2021 |
59. For scoring Data… physician performs an independent interpretation of an x-ray, a CT, and an MRI. He also orders a lab test. The physician did not bill for any of the tests interpreted. Strictly interpreting the data guidelines, it looks like Moderate. But it seems the physician is being penalized for performing 3 independent interpretations. If he only reviewed the reports on 2 of the scans, then he would have High data (1 independent interpretation, 2 tests reviewed and 1 test ordered). Can you clarify whether we can score High in this scenario?
The 2021 E/M changes are meant to reduce provider burden and offer the opportunity to choose the level of E/M service based on MDM or Total Time. The focus is the problems addressed at the encounter, the complexity of data reviewed and analyzed, and the patient management, rather than adding up a score.
Published |
02/xx/2021 |
60. Did Medicare change the allowed doctor able to bill a prolong code? We have Optometrists but do low vision rehab. Previously we were not able to obtain payment from Medicare for prolong service based on the provider type.
Optometrists, specialty 41, have the option to bill eye services or E/M service codes; however, they cannot bill for prolonged services. Optometrists should follow state regulations and apply with Medicare billing and coding guidelines.
Published |
02/xx/2021 |
61. On time for residents and the PCE. If a resident spends 15 min with pt and 5 min discussing with TP. Is the total time counted 20 min?
For the primary care exception, the teaching physician may direct the care furnished by the resident and review the services furnished by the resident during or immediately after the visit, remotely using audio/video real-time communications technology. When the resident and teaching physician collaborate, the time may only be counted once toward total time or total MDM.
Published |
02/xx/2021 |
62. Can you give examples when Ordering of Unique test can be counted under amount of complexity.
The order and review of a test (example, CBC) may be included when determining the level of service when the provider is not the billing entity.
Published |
02/xx/2021 |
63. I just want to clarify that CMS is NOT changing split/shared to allow it in the outpatient setting when "time" is used.
The AMA states, "A shared or split visit is defined as a visit in which a physician and other qualified healthcare professional(s) jointly provide the face-to-face and non-face-to-face work related to the visit.
When time is being used to select the appropriate level of a service for which time-based reporting of shared or split visits is allowed, the time personally spent by the physician and or other qualified health care professional(s) assessing and managing the patient on the date of the encounter is summed to define total time.
Only distinct time should be summed for shared or split visits (i.e., when two or more individuals jointly meet with or discuss the patient, only the time of one individual should be counted)." In the outpatient setting, this is referred as "incident to." After January 1, 2021, for office or other outpatient services, the provider may use MDM or total time when determining the E/M level of service.
Published |
02/xx/2021 |
64. The AMA specifies the interpretation and performance are not included in determining the levels of E/M services when the service is reported separately. It does not state that ordering the test is included in the determination of the levels of E/M services. Can it be explained why deciding to order a test should not be included in determining the level of E/M?
The Elements of Medical Decision Making table includes order and review of tests; therefore, they may be included when determining the level of service if the provider is not the billing entity.
Published |
02/xx/2021 |
65. My geriatric teaching physician has a telehealth visit (both audio and video) for a home visit patient. The patient is at home, and a resident is at the patient's home in person for this visit. How to bill this? Is code for home visit 99349 or charge code 99214 charged?
Appropriate modifier to be attached to charge with documentation of attestation as well.
Since the visit is originating from the home, CPT code 99349 would be used for the evaluation and management of an established patient, who requires at least two of the three components, a detailed interval history, detailed examination, and/or medical decision making of moderate complexity. Please see the 2021 CPT Book for additional coding elements to be met.
Published |
02/xx/2021 |
66. The CPT states in E/M 2021 guidelines under history/exam that information can be collected by the care team. Your fact sheet states that the HPI has to be documented by the billing provider/QHP. Can you clarify who can document the HPI under the new 2021 guidelines?
While the care team may collect information, the HPI must be documented by the physician or QHP. The AMA states, "Office or other outpatient services include a medically appropriate history and/or physical examination, when performed.
The nature and extent of the history and/or physical examination is determined by the treating physician or other qualified health care professional reporting the service.
The care team may collect information and the patient or caregiver may supply information directly (eg, by portal or questionnaire) that is reviewed by the reporting physician or other qualified health care professional.
The extent of history and physical examination is not an element in selection of office or other outpatient services."
Published |
02/xx/2021 |
67. Is recommending sunscreen considered a OTC treatment, and therefore low risk?
Sunscreen is considered straightforward on the Table of Risk; however, clear and concise documentation may support other consideration.
Published |
02/xx/2021 |
68. Where does referring a patient to another provider for a consult fall on the MDM chart?
A referral with discussion of management with an external physician/other QHP may fall under the Amount and/or Complexity of Data to be Reviewed and Analyzed.
The AMA states, "Referral without evaluation (by history, exam, or diagnostic study[ies]) or consideration of treatment does not qualify as being addressed or managed by the physician or other qualified health care professional reporting the service."
Published |
02/xx/2021 |
69. If the normal protocol for pulse ox is to perform as part of vitals, would this count as data for an ordered test?
No, if the pulse oximeter measurement is routinely assessed as part of a full set of vital signs, it is not considered an ordered test.
Published |
02/xx/2021 |
70. If we bill for a service (lab or imaging) under our TIN can we count it as order OR review? I know we can't as both. Example: Patient comes in and we order a PSA that is done in our office (so PSA 84153 is billed under our TIN) can we count that under the data section as Order of a unique test?
When the lab or imaging is performed and billed by your office, it cannot be included when selecting an E/M level of service. However, the physician may choose the level of service based on qualifying factors of Total Time.
Published |
02/xx/2021 |
71. If we bill the technical component for a CT scan under our TIN but we send to a radiologist that isn't associated with our TIN to read: 1. can we count that under review of a unique test OR independent interpretation of a test performed by other professional if we read the images ourselves or 2. If we just look at the report can we count that under review of a unique test.
If the provider is the performing and billing entity on a separately reported test, the ordering, review, and independent interpretation are not included when choosing an E/M level of service.
The AMA states, "The physician's interpretation of the results of diagnostic tests/ studies (ie, professional component) with preparation of a separate distinctly identifiable signed written report may also be reported separately, using the appropriate CPT code and, if required, with modifier 26 appended. If a test/study is independently interpreted in order to manage the patient as part of the E/M service, but is not separately reported, it is part of medical decision making."
Published |
02/xx/2021 |
72. Can the ordering of a point of care test be counted under Category 1, Data Reviewed/Analyzed?For example, patient comes into our urgent care site with a sore throat. A point of care strep test is ordered and reviewed by the provider. The test will be billed with the E&M. Can the provider receive credit under Category 1 for the ordering?
If the physician is the billing entity, they are already getting paid for that test separately and therefore it cannot be included in determining the level of E/M service based on MDM.
The AMA states, "When the physician or other qualified health care professional is reporting a separate CPT code that includes interpretation and/or report, the interpretation and/or report should not be counted in the medical decision making when selecting a level of office or other outpatient service."
Published |
02/xx/2021 |
73. Can a provider receive credit as independent interpretation of a test if they are the one ordering it? For example family medicine provider orders xray, reviews the image and documents the findings in the note. Is provider allowed to count the review of the xray image as independent interpretation? (Radiology will be billing for the technical and professional components.)
The provider may include the xray order and review in their MDM. The provider cannot include the independent interpretation since the radiologist is billing the professional component and will be providing the interpretation.
The AMA defines independent interpretation as: "The interpretation of a test for which there is a CPT code and an interpretation or report is customary. This does not apply when the physician or other qualified health care professional is reporting the service or has previously reported the service for the patient. A form of interpretation should be documented, but need not conform to the usual standards of a complete report for the test."
Published |
02/xx/2021 |
74. If a physician or QHP provider request to obtain medical records at the date of the encounter and if those records are not received until the day after the encounter and the patient does not return to review those with the provider can he or she can this as a unique source?
If choosing the E/M level of service based on MDM, the physician would need to review the requested medical records. If the records are received after the date of service, an addendum may be added to their documentation to include their review and how it was used in their MDM and treatment plan.
If choosing the E/M level of service based on Total Time, "obtaining and/or reviewing separately obtained history" is only included when performed on the date of the encounter.
Published |
02/xx/2021 |
75. If a physician or QHP is making a decision to refer a patient out to another external physician or QHP, however, is not having any discussion with that referring provider, only simply scheduling the appointment and giving the patient instructions, how does this count as MDM or is there any data points counted in this scenario?
The scenario provided does not qualify when choosing the level of service based on MDM as the physician would need to have discussed the referral or management with the external physician. Please note that the AMA states, "Referral without evaluation (by history, exam, or diagnostic study[ies]) or consideration of treatment does not qualify as being addressed or managed by the physician or other qualified health care professional reporting the service."
If choosing the level of service based upon Total Time on the date of the encounter, the AMA provides a specific list of qualifying activities.
References:
Published |
02/xx/2021 |
76. My question is regarding the portion of the MDM Complexity of Data, "Independent interpretation of tests". Are there recommendations of specific verbiage that have to be present in order to give the physician credit? For example, "I personally reviewed the XR and advise follow-up with an orthopedist, etc __ "
In the Urgent Care we have the following statement from the physician: Medical Decision Making 83-year-old male presents with some low back pain. X-ray lumbar spine shows no fracture but severe degenerative disease. Likely the patient's pain is secondary to this. I have encouraged him to try a Lidoderm patch which I will write for, alternating therapies with ice and heat. He has a scheduled appoint with his PCP tomorrow but deferred any further treatment of this to them. He is agreeable to plan was discharged home in stable condition.
The XR had a separate dictation from the Radiologist with this exact statement above – there is no additional information the physician provided outside of the radiologist interpretation.
The Urgent Care physician do not bill any professional component of the radiology service.
In your opinion, what type of documentation other than "I personally reviewed" should be present in the documentation for an Independent Interpretation?
The documentation should be clear and concise that the physician has independently interpreted the test or films including their findings and used this to determine the treatment plan.*
Please note, if the provider is the performing and billing entity on a separately reported test, the ordering, review, and independent interpretation are not included when choosing an E/M level of service.
The AMA states, "The physician's interpretation of the results of diagnostic tests/ studies (ie, professional component) with preparation of a separate distinctly identifiable signed written report may also be reported separately, using the appropriate CPT code and, if required, with modifier 26 appended. If a test/study is independently interpreted in order to manage the patient as part of the E/M service, but is not separately reported, it is part of medical decision making."
*We cannot provide information that could be construed as approval and would guarantee payment.
Published |
02/xx/2021 |
77. Let's say a practitioner orders a test during a prior visit but the patient does not obtain/perform the test, and then the patient is seen today for a subsequent visit. If the practitioner reorders the test, does that count as a data element for today's visit? If yes, what if the practitioner just advises the patient to obtain the previously ordered test without placing a new order?
The scenario posed has multiple unstated elements that affect the determination of level of service.
Technically, if the original order/review was included in determining the E/M level of service on the prior date, then it would not be included in the subsequent visit even if the same test needed to be reordered.
The provider may also use qualifying factors in Total Time on the date of the encounter when choosing the level of service.
Published |
02/xx/2021 |
78. Can you please provide a clear interpretation on the new E/M guideline with regards to crediting data elements- ordering a test is included in the category of test result(s) and the review is part of the encounter and not a subsequent encounter?
If a provider ordered a test during one visit and review the same test during the next visit, can the provider count this as a data point for both visits or not?
There are two arguments based on this language, some experts advise you'd credit both ordering and reviewing at the initial visit. In other words, it's assumed that if a provider orders a test, he or she intends to review it eventually. While others say the review should be credited on the subsequent visit, because the notes for that visit will indicate the review and discussion.
The AMA, which CMS has aligned with, clearly states, "Ordering a test is included in the category of test result(s) and the review of the test result is part of the encounter and not a subsequent encounter.
CGS interprets this direction as the order and review would be included on the same date of service when choosing E/M the level of service based upon MDM.
Published |
02/xx/2021 |
79. What does "Ordering a test is included in the category of test result and the review of the test result is part of the encounter and not a subsequent encounter" mean? I have seen people interpret this many different ways. How will CGS be 'counting' ordering and reviewing tests?
CGS will not be 'counting' items to fulfill a selected code; rather the focus is the care provided and clearly documented which is then evaluated to determine the level of service met.
CGS interprets the AMA's statement, which CMS has aligned with, as the order and review would be included on the same date of service when choosing the E/M level of service based upon MDM.
Published |
02/xx/2021 |
80. There have been questions that have come up regarding cardiac cath's. Since a minor/major surgery with or without risks is not determined by the global days any longer, what is recommended to make that determination?
(My providers are trying to determine where the risk would fall. They understand they need 2 of the 3 components but are struggling with a cath procedure and risk.)
The provider needs to assess and clearly document the patient's individual risk factors along with the procedure's risk factors to determine the overall risk. The risk determination is also based upon the "usual behavior" of a physician or QHP within that specialty.
Per the 2021 CPT Book Table of Risk, cardiovascular imaging studies with contrast and no identified risk factors (eg, arteriogram, cardiac catheterization) may be included in the moderate level of risk; whereas, cardiovascular imaging studies with contrast with identified risk factors may be included in a high level of risk.
The AMA defines risk as: "The probability and/or consequences of an event. The assessment of the level of risk is affected by the nature of the event under consideration. For example, a low probability of death may be high risk, whereas a high chance of a minor, self-limited adverse effect of treatment may be low risk. Definitions of risk are based upon the usual behavior and thought processes of a physician or other qualified health care professional in the same specialty. Trained clinicians apply common language usage meanings to terms such as 'high', 'medium', 'low', or 'minimal' risk and do not require quantification for these definitions, (though quantification may be provided when evidence-based medicine has established probabilities). For the purposes of medical decision making, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated. Risk also includes medical decision making related to the need to initiate or forego further testing, treatment and/or hospitalization."
Published |
02/xx/2021 |
81. I have a question, for Behavioral Health, when they check the OOARS report during the patient visit and make the patient aware of no suspicious activity, would this count as prior external note source reviewed? I was advised it's discussion of management or test interpretation, but I don't agree.
If the Rx history report is intentionally requested and used in the providers MDM, it may be considered a review of prior external notes from each unique source. If this is a routine order per state requirement, practice policy, etc., and it is not used in MDM it would not be considered.
Published |
02/xx/2021 |
82. Do you only get to take credit for 1 order and results review per CPT category (lab/rad/med) or is it per service with a CPT code? Example: 3 labs ordered at a visit that a separate entity will bill out with 3 different CPT codes out of the 8xxxx section of CPT (not a panel). Would a provider apply 3 orders and 3 results reviewed to achieve the Moderate level for Data or 1 order and 1 result reviewed to reach the Limited level?
HCPCS, ICD-10, and CPT are each a code set. The CPT code set then breaks down to sections such as Radiology, Pathology/Laboratory, or Medicine which CGS considers an individual "code set." Therefore, the 3 ordered laboratory tests would be included once.
The AMA defines test as: "Tests are imaging, laboratory, psychometric, or physiologic data. A clinical laboratory panel (eg, basic metabolic panel [80047]) is a single test. The differentiation between single or multiple unique tests is defined in accordance with the CPT code set."
Published |
02/xx/2021 |
83. With regards to presenting problems and complexity addressed, can you please give examples as to when to apply moderate versus high when the diagnosis is cancer?
The key words are complexity of problems addressed. A diagnosis of cancer has different variables such as type, stage and treatment plan that are considered along with any co-morbidities in a provider's medical decision making. The Table of Risk provides the following examples:
Published |
02/xx/2021 |
84. Prescription Drug Management- Can the provider get credit for this if they increase or decrease a medication in the new 2021 office guidelines?
Yes, prescription drug management includes a dosage increase or decrease (or addition of a new medication) based upon clear documentation of a problem addressed and data reviewed for patient management.
Published |
02/xx/2021 |
85. Would you please clarify, if a practitioner states that a prescription medication should be continued at the same dose and schedule for a chronic problem (e.g., Hypertension: Stable. Continue same dose of Lisinopril 20 mg by mouth daily.) is that considered prescription drug management in the MDM table column of "risk of complications and/or morbidity or mortality of patient management", moderate level?
No; the stable hypertension is at the treatment goal and the medication dosage did not change.
Published |
02/xx/2021 |
86. Reviewing medications and determining that the dose is correct and that continuing a medication is beneficial seems to be a service that should qualify as management. Can you please review and clarify why this would not meet the requirement?
The medical decision making to adjust any prescription medication when addressing and managing a problem or disease requires a higher complexity than refilling or continuing a medication; therefore, the documentation must be clear and concise when describing why a prescription medication was changed or continued. Simply providing a list of the patient's medications or stating 'reviewed' would not be considered prescription drug management complexity.
The provider may also choose to use qualifying factors of Total Time when choosing the E/M level of service.
Published |
02/xx/2021 |
87. I just wanted to clarify that Prescription Drug Management in the Moderate Row of the MDM chart does NOT include refills or continue current medication(s). It appears from the Q & A this would only include increasing or decreasing a medication or a new medication. Would you please clarify how a refill or continue current medication (without a refill being needed at that visit) would be considered by CGS?
Only documenting 'reviewed' on the medication list does not support Prescription Drug Management. Prescription drug management includes a dosage increase or decrease (or the addition of a new medication) based upon clear documentation of a problem addressed and data reviewed for patient management. If the provider is addressing a problem that includes continuing a prescription drug (or refill) in their education and medical decision making to manage the diagnosis, then it may be included in Prescription Drug Management.
The provider may also choose to use qualifying factors of Total Time when choosing the E/M level of service.
Published |
02/xx/2021 |
88. I just want to validate for the time in a Primary Care Exception clinic where the TP only has to review the care furnished by the residents during or immediately after each visit (the teaching physician may not see the patient); how would time be counted in that instance? We have received conflicting information from our various MACs.
For the primary care exception, the teaching physician may direct the care furnished by the resident and review the services furnished by the resident during or immediately after the visit, remotely using audio/video real-time communications technology. When the resident and teaching physician collaborate, the time may only be counted once toward total time or total MDM. The following resource provides the codes for E/M services the resident performs when the teaching physician is not present.
Reference: The MLN Booklet, Guidelines for Teaching Physicians, Interns, and Residents![]()
Published |
02/xx/2021 |
89. We are looking for guidance/clarification from CMS/CGS regarding billing for Resident (Physician) time under the E/M 2021 Guidelines.
Resident work is billed under the supervising/teaching physician's PTAN and must meet CMS regulations, coding, and billing guidelines. There are many variables and criteria that must be met, please see the following resources.
Published |
02/xx/2021 |
90. The question is: under the new 2021 E/M Guidelines, is the resident's time counted and combined with the teaching provider's time for total billing time?
Per the 42 CFR, § 415.172 Physician fee schedule payment for services of teaching physicians.
(a) General rule. If a resident participates in a service furnished in a teaching setting, physician fee schedule payment is made only if a teaching physician is present during the key portion of any service or procedure for which payment is sought. In residency training sites that are located outside a metropolitan statistical area, physician fee schedule payment may also be made if a teaching physician is present during the key portion of the service, including for Medicare telehealth services, through audio/video real-time communications technology for any service or procedure for which payment is sought.
42 CFR, § 415.174 Exception: Evaluation and management services furnished in certain centers. This exception for services furnished in outpatient departments of a hospital or another ambulatory care entity includes time spent by residents in patient care activities may be included in the level of service when specified conditions are met.
Published |
02/xx/2021 |
91. What is the appropriate prolonged service code to report with an outpatient consult service?
Please refer to the 2021 CPT Book for coding guidelines… "Consultation service codes may not be billed to Medicare for services rendered on or after January 1, 2010. Physicians must use visit/outpatient or inpatient hospital evaluation and management codes to bill Medicare for consultation services." A Medicare Cross-Walk from Consultation Codes to Outpatient/Hospital Codes table is available within the CPT book. Therefore, for office or other outpatient E/M services, the prolonged service code G2212 may be used when medically necessary and the visit meets the codes criteria.
The MLN Matters MM12071![]() includes the Total Time Required for Reporting G2212 (page 5).
includes the Total Time Required for Reporting G2212 (page 5).
Published |
02/xx/2021 |
92. Thank you for any insight you can give for support of a separate consult code with procedure code 95908 with a global indicator of XXX.
Per the National Correct Coding Initiative Policy Manual for Medicare Services, inherent pre-procedure, intra-procedure, and post-procedure work usually performed at the time of the procedure is completed is not reported as a separate E/M service. The consult note that was provided included the patient's chief complaint, history and exam related to the reason for the EMG (95908). There was no documentation to support any separate and significant service above the EMG.
E&M service may be related to the same diagnosis necessitating performance of the "XXX" procedure but cannot include any work inherent in the "XXX" procedure, supervision of others performing the "XXX" procedure, or time for interpreting the result of the "XXX" procedure. Appending modifier 25 to a significant, separately identifiable E&M service when performed on the same date of service as an "XXX" procedure is correct coding. National Correct Coding Initiative Policy Manual for Medicare Services, Chapter 4 https://www.cms.gov/files/zip/ncci-policy-manual-medicare-services-effective-january-1-2020.zip![]()
Please refer to the 2021 CPT Book for consult coding guidelines… "Consultation service codes may not be billed to Medicare for services rendered on or after January 1, 2010. Physicians must use visit/outpatient or inpatient hospital evaluation and management codes to bill Medicare for consultation services." A Medicare Cross-Walk from Consultation Codes to Outpatient/Hospital Codes table is available within the CPT book. Therefore, for office or other outpatient E/M services, the prolonged service code G2212 may be used when medically necessary and the visit meets the codes criteria.
Published |
02/xx/2021 |
93. When the Public Health Emergency (PHE) began, CMS issued directives that, for E/M services (99201-99215) conducted via telehealth through audio/video, the E/M level could be selected based on medical decision making or time through the end of the PHE. The times for these codes have changed with the implementation of the new 2021 guidelines. Since the PHE is still in effect, the question has arisen as to which times to use now for telehealth E/M services. For example, under 2020 times, a 99213 is met at 15 minutes. Under 2021 the time is 20-29 minutes. So which time should be used?
For dates of service on or after January 1, 2021, CMS has aligned with the AMA and providers should use the new guidelines for office or other outpatient services.
Published |
02/xx/2021 |
94. The name of the Medication is Fluorescein Sodium and it is a strip that is laid on the bottom of the eye lid and a drop of normal saline is dropped on the strip and it turns yellow.
Then a Cobalt light is used to shine in the patient's eye to check for any abrasions.
Our question is would this be considered part of or bundled into the E/M service?
This examination would be considered part of the E/M service as it is not a 'Special Ophthalmological Service'.
Published |
02/xx/2021 |
95. A practitioner performs an Annual Wellness Visit (AWV) and addresses the status of chronic problems. If all of the chronic problems are stable and considering the new 2021 office visit CPT guidelines:
May documentation of the stable chronic medical problems be used as elements in the American Medical Association's (AMA's) CPT medical decision making (MDM) table (see attached) as "number and complexity of problems addressed" for billing an evaluation and management (E/M) visit in addition to the AWV?
The AWV is a comprehensive assessment for medical (which includes chronic conditions) and family history, medications, cognitive assessment, depression screening, functional ability and safety, screening schedule for tests, list of risk factors and conditions, and educational and counseling programs.
If there is an acute or chronic problem identified during the AWV, which leads to an intervention that is significant, separately identifiable, and medically necessary additional work, a problem focused visit for that condition may be allowed with modifier 25 applied to the E/M billed and supportive documentation.
Modifier 25 (significant, separately identifiable evaluation and management [E/M] service by the same physician on the same day of the procedure or other service) sufficiently documented to support the claim for modifier 25 services.
Published |
02/xx/2021 |
96. May ordering and reviewing unique tests, reviewing prior external note(s) from each unique source, and/or assessment requiring an independent historian(s) for any stable chronic medical problems be counted as data elements in the AMA's CPT MDM table as "amount and/or complexity of data to be reviewed and analyzed" for billing an E/M visit in addition to the AWV?
Only the elements listed in your question would be applicable to the significant, separately identifiable evaluation and management [E/M] service relevant to an E/M with AWV. If there is an acute or chronic problem identified during the AWV, only the ordering and reviewing of unique tests, independent interpretation of tests you are not billing any component of, and a referral to another QHP with/or discussion of management or test interpretation with an external QHP may be allowed for billing the additional E/M with clear, concise, medically necessary documentation.
IOM 100-04, Chapter 12, Section 30.6.1.1; H. Reporting a Medically Necessary E/M Service Furnished During the Same Encounter as an IPPE or AWV.
When the physician or qualified NPP, or for AWV the health professional, provides a significant, separately identifiable medically necessary E/M service in addition to the IPPE or an AWV, CPT codes 99201 - 99215 may be reported depending on the clinical appropriateness of the circumstances. CPT Modifier -25 shall be appended to the medically necessary E/M service identifying this service as a significant, separately identifiable service from the IPPE or AWV code reported (HCPCS code G0344 or G0402, whichever applies based on the date the IPPE is performed, or HCPCS code G0438 or G0439 whichever AWV code applies).
NOTE: Some of the components of a medically necessary E/M service (e.g., a portion of history or physical exam portion) may have been part of the IPPE or AWV and should not be included when determining the most appropriate level of E/M service to be billed for the medically necessary, separately identifiable, E/M service. IOM 100-04, Chapter 12, Section 30.6.1
Published |
02/xx/2021 |
97. May documentation of the stable chronic medical problems be used to determine the "risk of complications and /or morbidity or mortality of patient management" in the AMA's CPT MDM table for billing an E/M visit in addition to the AWV?
When the physician or qualified NPP, or for AWV the health professional, provides a significant, separately identifiable medically necessary E/M service in addition to the AWV, CPT codes 99202 - 99215 may be reported depending on the clinical appropriateness of the circumstances. CPT Modifier -25 shall be appended to the medically necessary E/M service identifying this service as a significant, separately identifiable service from the AWV. Number and Complexity of Problem(s) Addressed, Amount and Complexity of Data Reviewed and Analyzed, and Risk of Complications and/or Morbidity or Mortality of Patient Management are elements of the 2021 E/M Components. https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf![]()
Published |
02/xx/2021 |
98. May total time be used to bill an E/M visit in addition to the AWV if the total time for the stable chronic medical problems used to determine the E/M visit is carved out from the AWV total time? If so, which of the following may be included when determining the carved out total time for the E/M visit?:
Yes, total time or MDM may be used to determine the E/M level of service. Only the components above that relate to the problem/diagnosis that is significant, separately identifiable medically necessary service(s) you are treating at the time of the AWV will be applied to the E/M billed.
If you use total time to level the E/M visit, along with an AWV, you will need to carve out the total time for the office visit specifically in the note. Example (for billing 99213-25 and G0439): A total of 45 minutes was spent on this visit, with 25 minutes spent on performing a physical exam, counseling the patient on managing DM and HTN, refilling medications and ordering labs for monitoring chronic disease.
Published |
02/xx/2021 |